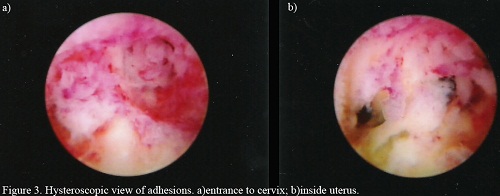
Ashermans Syndrome or AS is a rare condition affecting the uterus. Usually it occurs in women that have undergone several dilatation and curettage (D&C) procedures. Surgery to treat severe pelvic infection that is unrelated to the condition may also lead to Ashermans Syndrome the condition is characterized by tissue scarring inside the uterus and the cervix. Such scarring may cause the walls of the uterus to stick together.
Ashermans Syndrome, image Wikipedia
The symptoms of Ashermans Syndrome which involves breaking up the scar tissue and preventing re-growth of scar tissue can cause amenorrhea (lack of menstrual periods), hypomenorrhea (menstrual irregularities such as very light periods), pelvic discomfort or pain, repeated miscarriages, and infertility. Women who are infertile because of AS may have successful pregnancy if they get treated, depending on the severity of AS and the difficulty of the treatment.
Because it is undetectable through regular diagnostic procedures, AS is believed to be widely under-diagnosed. The normal method of diagnosis is a pelvic exam in addition to a blood test to detect tuberculosis or schistosomiasis and a transvaginal ultrasound examination.
To avoid this painful and debilitating condition, studies suggest that the avoidance of medical instrumentation in the uterine area is beneficial. A recent study showed that women who were treated for missed miscarriage with misoprostol did not develop AS whereas 7.7% of those who had a D & C procedure did develop the condition. In addition it appears that D & C operations that are guided by ultrasound and not performed blindly are less likely to result in AS as the surgeon is less likely to scrape the lining of the uterus during the procedure.
Treatment of AS is very specialized and requires the skills of a surgeon expertly trained to perform the procedure. All energy sources inside the uterus should be avoided. This complicates the procedure, requiring that the surgeon must rely on scissors to remove scars rather than lasers. A splint or balloon may be applied post-operatively to prevent reattachment of the uterine walls. To prevent re-scarring after a successful procedure, estrogen supplementation may be prescribed. Some surgeons also recommend weekly hysteroscopy for a period of weeks following the surgery to remove any post-operative adhesions that have formed.
AS, if left untreated, may result in infertility, miscarriage, intrauterine growth restriction and placenta accrete. In addition, the scarring of the uterus may lead to complete destruction of the uterine lining or cervical obstruction. This, in turn, may cause menses to be retained in the uterus. Feelings of severe pain in the pelvic area will result. The flow of menses into the abdominal cavity may lead to Endometriosis.
Women who have had a gynecologic or obstetrical procedure and have not returned to normal menstrual periods may have developed scarring as a result of their procedure. They should consult their medical professional for an examination. Those who have been unable to get pregnant after 12 months of trying should, likewise, have themselves checked for AS.
Related post :
1. Tubes Tied (Blocked Fallopian Tubes)
2. The Symptoms Of Ovarian Cyst


 Saving...
Saving...